Food poisoning caused by pathogenic agents is one of the major public health problems worldwide. Among the most frequent poisonings is Salmonellosis, a zoonotic infection that causes high rates of mortality and morbidity in almost all countries [1-3].
Salmonellosis is caused by Salmonella, a gram-negative rod-shaped (also known as bacillus) bacterium that can move using flagella or remain immobile. This bacterium belongs to the Enterobacteriaceae family, and is a facultative anaerobic bacterium, meaning that it uses oxygen to produce energy, it can also carry out anaerobic processes such as fermentation when oxygen is not available.
Salmonella can survive due to its great resistance under adverse conditions: [4,5]
- pH: survive at pHs ranging from about 4.0 to 9.5, however, the ideal pH range for growth of this bacteria is between 6.5 and 7.5.
- Temperature: optimal growth temperature between 35°C and 37°C, but can survive at very low temperatures, such as in frozen foods, and at very high temperatures, such as in foods subjected to high temperatures for a short period of time (e.g. during rapid cooking).
- Water activity (aw): environments with low water activity, such as in dry or dehydrated foods.
- High salt concentration: foods with high salt concentration, such as salted meats and canned foods.
- Biofilms: Salmonella is capable of forming biofilms on surfaces, which gives it greater resistance to antimicrobial agents (disinfectants and sanitizers) and allows for its survival for long periods of time.
Salmonella is present in the intestinal tract of both infected animals and humans, and the bacteria is typically excreted in feces. Contamination of water and food products with Salmonella occurs when food products come into contact with animal feces, usually due to inadequate hygiene practices in equipment, surfaces, or other materials used in food processing, whether in an industrial or domestic environment.
The most commonly affected foods include meat, milk, and eggs (where contamination can occur both on the shell and inside), as well as fruits, herbs, and spices during cultivation. In environments such as hospitals, nursing homes, and kindergartens, fecal-oral transmission of the bacteria can occur due to inadequate personal hygiene practices.
After ingestion of contaminated food or water, the symptoms can appear within a period of 6 - 72 hours (usually 12 - 36 hours), and illness lasts 2–7 days. The severity of symptoms varies but is more intense in the elderly, children, and individuals with weakened immune systems. Common symptoms include fever, diarrhoea, vomiting, and nausea [5,6].
Preventative measures for Salmonella spp. contamination
Both food producers and consumers should take measures to reduce the risk of Salmonella contamination in food, namely:
Producers:
- Having adequate sanitation and keeping septic tanks away from food production areas;
- Washing hands frequently and using protective equipment such as gloves and masks;
- Strict practices of food hygiene and safety, including frequent cleaning and disinfection of equipment and work surfaces, temperature control of storage, and proper cooking of foods;
- Vaccinating animals against Salmonella to reduce the incidence of the bacteria in their products, as the bacteria can be transmitted to humans through the consumption of contaminated animal-origin foods.
Consumers:
- Wash hands especially after using the bathroom, after touching animals, before meals and preparing them;
- Food hygiene: wash thoroughly raw foods that will be consumed (fruits, vegetables and greens) and avoid consuming undercooked animal products (especially meats and eggs);
- Consume boiled or pasteurized milk;
- Keep food stored at the proper temperature to prevent bacterial growth;
- Check the expiration date of foods before consuming them.
Importance of Microbiological Testing for Salmonella spp.
To ensure food safety, it is crucial for food producers to conduct microbiological tests throughout all stages of production, from sourcing raw materials to the final product, in addition to the previously mentioned control measures, to detect the presence of Salmonella spp.
Regarding raw materials, it’s crucial for the supplier to provide a certification that confirms the absence of Salmonella spp. When it comes the processing stage, it is necessary to perform testing at various critical points to ensure the effectiveness of quality control and food safety measures, including water, surfaces equipment, and the monitoring of the production environment. Furthermore, it is also necessary to carry out tests on samples of the final product, before it is distributed for consumption.
Tests that help identify possible Salmonella spp. contamination risks include total aerobic and anaerobic counts (to determine the total bacterial count present in a food), environmental monitoring (to evaluate the effectiveness of hygiene and cleaning programs in the production environment) and process validation (to assess the effectiveness of manufacturing processes). However, these tests are not specific to Salmonella spp. and can produce false negative results.
The most common specific tests for Salmonella spp. are the selective culture method and the real-time polymerase chain reaction (PCR) technique.
The selective culture method is usually performed on XLD agar (Xylose Lysine Deoxycholate), where Salmonella spp. colonies appear as red with a black center. However, this method has limitations, including (i) selectivity issues, where other bacteria may interfere with the results, leading to false positives or negatives; (ii) time: this method requires at least three days to be completed, making problematic in public health; situations where quick action is necessary to prevent outbreaks of foodborne illnesses; (iii) difficulty in complex cultures: In food samples with a large number of microorganisms, it may be difficult to isolate and identify Salmonella spp. using culture media as other microorganisms present may compete for space and nutrients [1].
The Real-time PCR technique is a highly sensitive and specific method that overcomes the limitations of other Salmonella spp. detection methods, including the culture method. It is capable of detecting even low levels of the bacteria in a short amount of time, typically within a few hours [7].
Salmonella spp. Detection with Real-Time PCR kits
- BPMR kits take full advantage of real-time PCR to enable a quick and reliable method for Salmonella spp. bacteria detection.
- These kits are based on gene amplification and detection using real-time PCR with an DNA-based assay.
- Ready-to-use PCR reagents contain everything required to detect targeted organisms with high sensitivity and specificity.
- The REAL TIME PCR DETECTION TEST KIT Salmonella spp. allows the detection of one target, the Salmonella spp. bacteria.
- All the kits also include an internal control (IC) that allows the exclusion of false negative results.
- Our kits have incorporated a Hot Start polymerase to enable reliable PCR amplification. The mix offers highly reproducible DNA synthesis.
Various tests were performed to ensure both kit quality such as inclusivity, sensitivity, and exclusivity:
- Inclusivity: A total of 50 Salmonella spp. strains were tested. All target strains tested with the kits were detected corresponding with 100% inclusivity.
- Sensitivity: Target amplification was observed in samples contaminated with 1-10 cfu/25 g or more.
- Exclusivity: More than 30 non-target microorganisms were tested with the kits showed 100% exclusivity with no positive results.
- For DNA extraction, our BIOPREMIER DNA Extraction from Food kit allows efficient extraction and purification of DNA samples from challenging matrices containing high levels of polyphenols. Furthermore, the purified DNA products can be used directly on the PCR.
BPMR present to you a global solution from the extraction and purification DNA of Salmonella spp. from food samples to its detection using our qPCR kits
Important advantages!
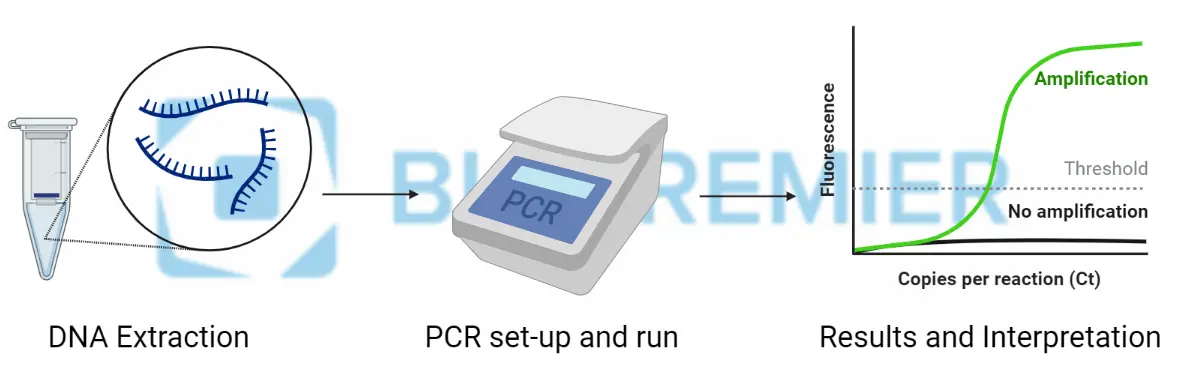
- Quick results (one-two days) in few steps: first Bacterial DNA Purification, followed by Pathogen Detection and lastly Data Analysis. Check below the “A simple Three-step Protocol”
- Accessible and easy to use thanks to a ready-to-use kits.
- Harmonized protocols for Real Time PCR detection.
- Compatible in the most used real time PCR equipment’s.
- Includes Positive and Negative PCR controls and Internal control.
Real-Time PCR Solution: A Simple Three-Step Protocol
This flexible and sturdy protocol fits smoothly in any analytical lab workflow to reach the best productivity! Ranges from low to high throughput testing, with simple to use user interface, to, in the end, provide efficient sample interpretation.
For more info and order request, the link for the kit below:
Real Time PCR Detection Test Kit Food Safety Salmonella Spp.
References:
[1] Awang MS, Bustami Y, Hamzah HH, Zambry NS, Najib MA, Khalid MF, Aziah I, Abd Manaf A. Advancement in Salmonella Detection Methods: From Conventional to Electrochemical-Based Sensing Detection. Biosensors (Basel). 2021 Sep 18;11(9):346. doi: 10.3390/bios11090346. PMID: 34562936; PMCID: PMC8468554.
[2] Ehuwa O, Jaiswal AK, Jaiswal S. Salmonella, Food Safety and Food Handling Practices. Foods. 2021 Apr 21;10(5):907. doi: 10.3390/foods10050907. PMID: 33919142; PMCID: PMC8143179.
[3] Paniel N, Noguer T. Detection of Salmonella in Food Matrices, from Conventional Methods to Recent Aptamer-Sensing Technologies. Foods. 2019 Sep 1;8(9):371. doi: 10.3390/foods8090371. PMID: 31480504; PMCID: PMC6770675.
[4] Tajkarimi M. Salmonella spp. 2007. Available at: https://www.cdfa.ca.gov/ahfss/Animal_Health/PHR250/2007/25007Sal.pdf
[5] https://www.who.int/news-room/fact-sheets/detail/salmonella-(non-typhoidal)
[6] https://www.asae.gov.pt/seguranca-alimentar/riscos-biologicos/salmonella
[7] Kasturi KN, Drgon T. Real-Time PCR Method for Detection of Salmonella spp. in Environmental Samples. Appl Environ Microbiol. 2017 Jun 30;83(14):e00644-17. doi: 10.1128/AEM.00644-17. PMID: 28500041; PMCID: PMC5494621.


