What is Legionella?
Legionnaire's Disease, caused by Legionella pneumophila bacteria, is a severe illness. In Portugal, this bacterium was first detected in 1979 and is listed as a mandatory reportable disease.
Legionella pneumophila is a Gram-negative bacterium that is dispersed in the environment and typically resides in water reservoirs such as rivers, lakes, springs, hot springs, and humid soil. Under favorable environmental conditions, this bacterium can rapidly multiply, leading to abnormal levels in water circulation and supply systems. The primary factors contributing to its growth include the presence of heat (optimal growth between 32ºC-40ºC within a range of 20-50ºC), stagnant water, and nutrient/residue availability.
This bacterium can be dispersed into the air, such as through mist or aerosolization from those water sources. Once airborne, it poses a risk to human health as an intracellular facultative pathogen that can utilize the eukaryotic cells of alveolar macrophages for its multiplication. In the environment, frequently associates with protozoa such as Amoeba, utilizing their eukaryotic cells for its multiplication. This association not only facilitates the bacterium's replication but also provides a protective environment, particularly against disinfectants.
Legionella pneumophila, the most clinically significant species, encompasses 15 serogroups. Among them, serogroups 1, 4, and 6 are responsible for 80-90% of human infections. Serogroup 1 Legionella pneumophila is commonly found in most patients diagnosed with Legionnaire's Disease. (1)
Legionnaire's Disease
In 1976, a congress in the USA resulted in an unexpected death toll of 34 people and severe pneumonia in 221 individuals. This event increased interest in Legionella, as the infection occurred due to favorable conditions for bacterial growth in the air vent system of the congress room.
In Portugal, Legionella was discovered in 1979 and is included in the mandatory declaration list of transmittable diseases. In 2004, a new program for epidemiological surveillance of Legionnaire's Disease was established to strengthen monitoring efforts.
Legionnaire's Disease is the most frequent and severe form of the illness, characterized by pneumonia as the primary symptom. Legionella pneumophila is the main causative agent, accounting for 90% of cases. Patients commonly experience high fever, anorexia, generalized myalgia, dry coughs, thoracic pain, diarrhea, and vomiting during the initial stages of the illness. (1)
Where can it be found
The natural habitat of Legionella are water reservoirs such as rivers, lakes, springs, hot springs, and humid soil. They can also be found in artificial systems of water circulation such as sanitary hot water circuits (showers), cold water circuits for human consumption, sprinkler irrigation, filters of A/C equipment and their conducts, refrigeration systems, dehumidifiers, nebulizers, and decorative fountains. (1)
Transmission sources
Exposure to Legionella may not lead to infection. The infection depends on the level of water contamination, dissemination efficiency of bacteria through air, the human host’s characteristics, and the virulence of Legionella strain. Most of the cases of infection (80%) are sporadic without a known reservoir and the other 20% are within the context of outbreaks.
The infection is transmitted airborne, through inhalation of contaminated water drops and is not transmitted by consumption of contaminated water or from people to people.
The capability of Legionella accessing the respiratory tract is initially related to the size of the inhaled aerosol. Aerosols with a diameter bigger than 10 µm are retained on the nose and throat; aerosols between 5-10 µm can reach the superior and inferior respiratory tract; aerosols even smaller between 2-5 µm can reach the lungs and airways. The incubation period may vary between 2 to 14 days (frequently 3-6 days). (1)
Risk groups
Not every individual exposed to the bacteria develops the disease. This disease is rare in children on teenagers below 20 years old. The immune system alone may be sufficient to combat bacteria and avoid infection. The disease affects mostly male individuals, smokers, alcoholism, immunodepressive and chronic diseases and people above 30-40 years old or when immune system defenses are low, and susceptible to infection after contact with the microorganism.
Patients doing treatment in chemotherapy or corticoids, with chronical breathing diseases, such as asthma or COPD (Chronic Obstructive Pulmonary Disease) and elderly people have a great risk once in contact with bacteria that may lead to serious pneumonia cases, which can end with death.
Legionella infection in hospitals may occur due to several risk factors: recent surgery, intubation, mechanical ventilation, aspiration, presence of nasogastric waves and use of equipment for respiratory therapy. (1)
How to proceed with Legionella infection
If symptoms are present and exposure to aerosol of dubious quality, especially if there are known cases in the same area. Health authorities must be informed to report these cases before contacting a local doctor or hospitals.
Diagnosis
Various samples can be taken from various secretions of the respiratory tract, including sputum. Frequently the sputum exhibits purulent characteristics, often with an aqueous consistency or containing blood.
Bacterial growth can be performed using media with adequate nutritive supplements (BCYE media) and longer incubation periods (5-10 days). The culture exam has the advantage of allowing the comparison of clinical isolates with environmental isolates.
qPCR is a good method for the diagnosis of Legionella. It enables rapid detection, allowing for timely intervention and treatment and provides high sensitivity and specificity, ensuring reliable and accurate results for effective management of Legionella infections.
For serological analysis, an increase of 4 times on the concentration of antibodies anti-Legionella, in serum collected with more than 2 weeks of interval can be used for retrospective diagnosis of Legionella.
Direct immunofluorescence can be performed directly on biological samples on a quick way with 95% specificity but only 25-75% sensitivity. (1)
Treatment
Treatment for Legionnaire's Disease involves the administration of antibiotics. Antibiotic treatment is necessary for patients with pulmonary symptoms, while non-pulmonary patients do not typically require antibiotics. Prompt initiation of therapy based on examination results is essential.
The recommended antibiotics for Legionnaire's Disease are macrolides (azithromycin or clarithromycin), quinolones (levofloxacin or moxifloxacin), tetracyclines (doxycycline), or rifampicin. Levofloxacin, considered a first-line antibiotic, has shown better activity compared to macrolides. In severely ill patients, rifampicin may not be necessary when using doxycycline or fluoroquinolones.
The duration of treatment (5 days to 3 weeks) may vary depending on the patient's condition and the chosen antibiotic. (1)
Legionella Detection in water sources
Test methods for risk assessment may be varied depending on the water system and the reason for testing.
Traditional culture methods (spread plate):
Culture testing is the traditional method for detecting Legionella bacteria in water sources. It involves allowing a sample of bacteria to grow in a controlled environment until it becomes visible for analysis. However, relying solely on culture testing has drawbacks. The process is time-consuming, taking up to two weeks, which delays confirmation of Legionella presence during disease outbreaks. Specialized equipment and personnel are needed for accurate culturing, and Legionella's growth within biofilms further complicates the process by hindering accurate detection on petri dishes.
Characteristics of Culture plate method:
- Growth of viable bacteria of all Legionella species.
- Results are typically presented in cfu/mL with a detection limit of approximately 10 cfu/mL
- Produce isolates for further characterization.
- Results reported between 7-14 days.
- Depends on the experience, know-how and rigor of the laboratory.
- Preferred for evaluation of growth trends.
Quantitative Polymerase Chain Reaction (qPCR):
Recent advancements in biotechnology have introduced a faster and more accurate method for detecting Legionella bacteria called qPCR testing. Unlike culture testing, which involves growing bacteria, qPCR testing isolates the bacteria's DNA from a water sample. This allows for the detection of Legionella without the need for culturing, providing results in under two hours. qPCR testing can also identify viable but non-culturable bacteria, offering a more comprehensive assessment of risk. Dormant bacteria that may not grow in a petri dish can still be detected through qPCR testing since their DNA remains present.
Characteristics of qPCR:
- Detects Legionella specific DNA;
- May not differentiate between live or dead bacteria.
- Results usually reported in genomic units (GU) which is not a direct equivalent to cfu
- Results reported very fast – between 2-48 hours
- Can be useful for negative screening.
- Preferred for evaluating whether remediation was successful.
How to prevent Legionella spread
Since Legionella is capable of surviving for long period of time in hostile environmental conditions, the human being has a bigger risk of being exposed to this agent. Since it’s a bacteria hard to prevent, it’s important a periodic check on the water systems and the refrigeration systems of the buildings, being these the focal points of infection.
Various procedures for Legionella elimination:
- Physical operations – Controlling water temperature (maintaining temperatures below 20ºC or above 60ºC), promoting vapor production and utilizing ultraviolet disinfection.
- Chemical – Employing chlorine and its derivatives, utilizing others agents such as bromine (Br), copper ionization (Cu2+) and silver (Ag+).
- Employing biocidal products, anti-corrosive agents, and descalers is essential in mitigating the risk of Legionella contamination.
- Promote periodically detection of Legionella bacteria (1)
In home settings, we can take some preventive measures to reduce the risk of Legionella contamination:
- Avoiding inhaling water vapors of showers, pools, jacuzzis, or other places that hygiene may look dubious or unknown or if you belong to a risk group.
- Periodically set your water heater to heat up to over 60ºC for a set period of time to kill any bacteria that may be growing.
- Cleaning the filters of faucets and dip the “heads” of the showers in bleach, with the care of rinsing them very well after cleaning.
- Avoid inhaling the initial vapors emitted from stagnant water sources such as water heaters or gas heaters. (2)
Legionella detection with Real-Time PCR kits
- BPMR kits take full advantage of real-time PCR to enable a quick and reliable method for Legionella spp. and Legionella pnemophila bacteria detection.
- These kits are based on gene amplification and detection using real-time PCR with an DNA-based assay.
- Ready-to-use PCR reagents contain everything required to detect targeted organisms with high sensitivity and specificity.
- The REAL TIME PCR DETECTION TEST KIT Legionella spp. allows the detection of the target, the Legionella spp. bacteria.
The REAL TIME PCR DETECTION TEST KIT Legionella pnemophila allows the detection of one target, the Legionella pneomophila bacteria.
- All the kits also include an internal control (IC) that allows the exclusion of false negative results.
- Our kits have incorporated a Hot Start polymerase to enable reliable PCR amplification. The mix offers highly reproducible DNA synthesis.
Various tests were performed to ensure both kit quality such as inclusivity, sensitivity, and exclusivity:
- Inclusivity: A total of 30 Legionella spp strains were tested. All target strains tested with the kits were detected corresponding with 100% inclusivity.
- Sensitivity: Target amplification was observed in samples contaminated with at least 103-104 cfu/1 L for both Legionella spp. and Legionella pneumophila.
- Exclusivity: A total of 30 non-target microorganisms were tested with the kits showed 100% exclusivity with no positive results.
- For DNA extraction, our BIOPREMIER DNA Rapid Extraction Buffer allows efficient extraction and purification of DNA samples. Furthermore, the purified DNA products can be used directly on the PCR.
BPMR present to you a global solution from the extraction and purification DNA of Legionella spp. and Legionella pneumophila from water samples to its detection using our qPCR kits
Important advantages!
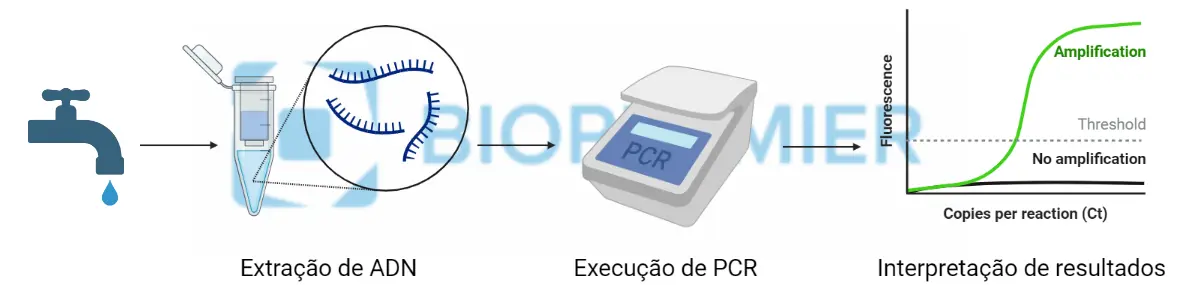
- Quick results (one-two days) in few steps: first Bacterial DNA Purification, followed by Pathogen Detection and lastly Data Analysis. Check below the “A simple Three-step Protocol”.
- Accessible and easy to use thanks to a ready-to-use kits.
- Harmonized protocols for Real Time PCR detection.
- Compatible in the most used real time PCR equipment’s.
- Includes Positive and Negative PCR controls and Internal control.
Real-Time PCR Solution: A Simple Three-Step Protocol
This flexible and sturdy protocol fits smoothly in any analytical lab workflow to reach the best productivity! Ranges from low to high throughput testing, with simple to use user interface, to, in the end, provide efficient sample interpretation.
Created with BioRender.com
REAL TIME PCR DETECTION TEST KIT Legionella spp.: click here
REAL TIME PCR DETECTION TEST KIT Legionella pneumophila: click here
REAL TIME PCR DETECTION TEST KIT Legionella duplex: click here
References:


