Listeria monocytogenes is described as a ubiquitous pathogenic bacteria, majorly responsible for isolated cases and outbreaks of listeriosis in humans and animals. When it first was discovered, it was only recognized as being dangerous to animals. Later in the 80s, due to several outbreaks of bacteria-contaminated food, this bacteria were seen as a threat to public health.
L. monocytogenes is a type of Gram-positive bacteria that belongs to the family Listeriaceae. This bacteria can grow both in the presence and absence of oxygen and is considered a facultative anaerobe. L. monocytogenes has rod-shaped cells that are motile due to the presence of flagella.
L. monocytogenes bacteria thrive under specific conditions including temperature ranges of -0.4°C to 45°C, with optimal growth between 30°C and 37°C. They can survive in frozen food for extended periods however can be eliminated from milk through pasteurization. These bacteria can grow in environments with pH values between 4.3 and 9.4 and tolerate a minimum water activity (AW) of 0.92, as well as 10% NaCl. Anaerobic conditions promote their growth, while CO2 concentrations exceeding 80% are inhibitory (1).
Foods associated with L. monocytogenes infections
Contamination sources of Listeria monocytogenes include soil, water, food processing environments, raw and processed foods, animal reservoirs, cross-contamination, and improper storage and handling. The bacteria L. monocytogenes can be found ubiquitously on the ground, vegetables, meat, and fish, and can be carried asymptomatically by both animals and humans. Consequently, raw materials and non-processed foods are frequently contaminated. The risk of contamination is particularly high in products that do not undergo any reduction or elimination stage during the manufacturing process, and whose raw materials have a higher incidence of bacteria. Examples of susceptible foods include salads, pâtés, cheeses, pasteurized milk, shrimp, and butter. Moreover, the bacteria's rapid growth rate and lack of processing before consumption increase the contamination risk in products like raw milk, raw milk derivatives, smoked fish, and certain sausages (1).
Contamination prevention and protection
Ensuring the complete absence of L. monocytogenes is not feasible as it can be found in food, particularly thermally processed foods, indicating poor hygiene practices. To prevent contamination and cross-contamination, maintaining good hygiene and manufacturing practices is crucial. Implementing self-control systems like HACCP (Hazard Analysis and Critical Control Points) throughout the production chain is essential to prevent outbreaks.
To protect against Listeria infection, it is important to be aware of risky foods and avoid them:
- Raw (unpasteurized) milk and soft cheeses made from it, including pasteurized milk Mexican-style cheeses like queso fresco, have been linked to Listeria infections due to contamination during cheese-making.
- Deli meats and hot dogs should be thoroughly heated before consumption.
- Leftovers should be promptly refrigerated in covered, shallow containers and consumed within 3-4 days.
- Avoid cross-contamination in the kitchen.
- Maintain the refrigerator at a temperature of 4ºC or lower and the freezer at -18ºC or lower (2).
To prevent Listeria contamination, follow these steps:
- Wash the inside walls, shelves, cutting boards, and utensils of the refrigerator with hot water and soap, then sanitize them with a chlorine bleach solution diluted in hot water.
- Immediately clean up spills and regularly clean the refrigerator.
- Wash hands with warm water and soap for at least 20 seconds before and after handling food or engaging in any cleaning and sanitation procedures (22).
Certain groups, such as pregnant women, the elderly, and individuals with weakened immune systems, should avoid high-risk foods including unpasteurized/raw milk, cheeses made from unpasteurized milk, raw fish, raw sprouts, and other raw foods that pose a high risk of L. monocytogenes contamination. Pet owners should take precautions to prevent cross-contamination when handling their pet's food. Food dishes should be promptly washed after pets finish eating, and individuals with weakened immune systems should avoid handling or being exposed to potentially contaminated food or pets.
In the event of possible exposure to L. monocytogenes, it is important to contact the local health department and communicate with customers. Display cases and surfaces used to store, serve, or prepare potentially contaminated foods should be regularly washed and sanitized. Cutting boards and utensils used in food processing should also be frequently cleaned and sanitized to minimize the risk of cross-contamination. Consumers can play a role in preventing future outbreaks by voluntarily reporting complaints or adverse events (illnesses or serious allergic reactions) related to food products.
Listeria monocytogenes detection
Plate culture method is one of the selection methods of Listeria monocytogenes detection. Food samples typically contain damaged cells, so a nonselective pre-enrichment step is often needed before selective enrichment and isolation on selective/differential agar media. Negative results from plating can take 3-4 days to be confirmed, while positive results may take 5-7 days (3).
Even with enrichment, detection can be challenging due to factors like a high population of competitive microbiota, low levels of the pathogen, and interference from inhibitory food components. In addition, false negatives may occur when L. innocua grows faster than L. monocytogenes on a commonly used culture medium that does not differentiate between them (3).
An alternative to culture method is PCR detection
For a faster, efficient, and effective analysis, qPCR strategy is crucial. The analysis can take 1-2 days, with the sample preparation being the most time-consuming step. The most used method is enrichment culture, which involves a pre-enrichment step using the non-selective medium of the cultural method. Enrichment culture allows for the growth of a single damaged cell to levels of 103 cfu/mL, enabling its detection through PCR (4).
In BPMR, we advise the detection of this pathogen using our REAL TIME PCR DETECTION TEST KIT Listeria monocytogenes for accurate, reliable and quick detection of this pathogen in your sample, reducing costs in loss of raw materials or by preventing outbreaks from occurring .
Listeria monocytogenes Detection with Real-Time PCR kits
- BPMR kits take full advantage of real-time PCR to enable a quick and reliable method for Listeria monocytogenes bacteria detection.
- These kits are based on gene amplification and detection using real-time PCR with an DNA-based assay.
- Ready-to-use PCR reagents contain everything required to detect targeted organisms with high sensitivity and specificity.
- The REAL TIME PCR DETECTION TEST KIT Listeria monocytogenes allows the detection of one target, the Listeria monocytogenes bacteria.
- All the kits also include an internal control (IC) that allows the exclusion of false negative results.
- Our kits have incorporated a Hot Start polymerase to enable reliable PCR amplification. The mix offers highly reproducible DNA synthesis.
Various tests were performed to ensure both kit quality such as inclusivity, sensitivity, and exclusivity:
- Inclusivity: A total of 23 Listeria monocytogenes strains were tested. All target strains tested with the kits were detected corresponding with 100% inclusivity.
- Sensitivity: Target amplification was observed in samples contaminated with 1-10 cfu/25 g or more.
- Exclusivity: A total of 30 non-target microorganisms, including Listeria innocua, were tested with the kits showed 100% exclusivity with no positive results.
- For DNA extraction, our BIOPREMIER DNA Extraction from Food kit allows efficient extraction and purification of DNA samples from challenging matrices containing high levels of polyphenols. Furthermore, the purified DNA products can be used directly on the PCR.
BPMR present to you a global solution from the extraction and purification DNA of Listeria monocytogenes from food samples to its detection using our qPCR kits
Important advantages!
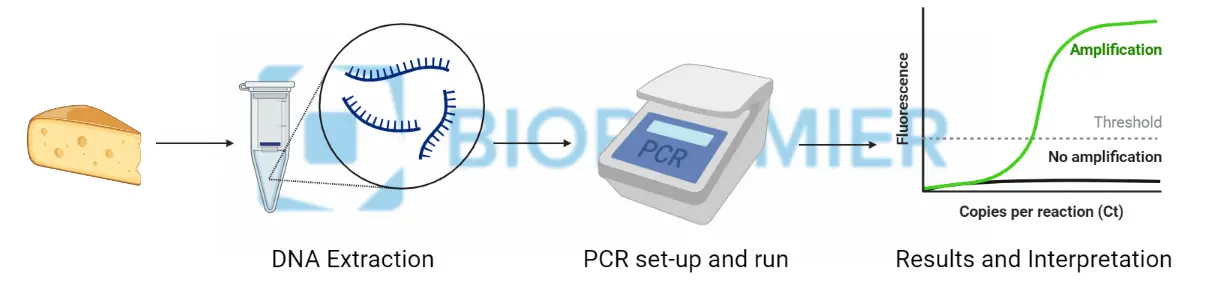
- Quick results (one-two days) in few steps: first Bacterial DNA Purification, followed by Pathogen Detection and lastly Data Analysis. Check below the “A simple Three-step Protocol”
- Accessible and easy to use thanks to a ready-to-use kits
- Harmonized protocols for Real Time PCR detection
- Compatible in the most used real time PCR equipment’s
- Includes Positive and Negative PCR controls and Internal control
Real-Time PCR Solution: A Simple Three-Step Protocol
This flexible and sturdy protocol fits smoothly in any analytical lab workflow to reach the best productivity! Ranges from low to high throughput testing, with simple to use user interface, to, in the end, provide efficient sample interpretation.
REAL TIME PCR DETECTION TEST KIT Listeria monocytogenes: click here
References:
1- https://www.asae.gov.pt/seguranca-alimentar/riscos-biologicos/listeria-monocytogenes
2- https://www.fda.gov/food/foodborne-pathogens/listeria-listeriosis
3- Mester, P., Witte, A. K., & Rossmanith, P. (2021). Sample Preparation for qPCR Detection of Listeria from Food. Methods in molecular biology (Clifton, N.J.), 2220, 31–40. https://doi.org/10.1007/978-1-0716-0982-8_3
4- Witte, A. K., Mester, P., & Rossmanith, P. (2021). qPCR Validation on the Basis of the Listeria monocytogenes prfA Assay. Methods in molecular biology (Clifton, N.J.), 2220, 41–53. https://doi.org/10.1007/978-1-0716-0982-8_4


